Sleep Apnea
What is the difference between home sleep test vs sleep test in a sleep clinic?
A home sleep test and a sleep test conducted in a sleep clinic are both diagnostic tools used to evaluate sleep disorders such as sleep apnea. However, there are some key differences between the two:
Setting: The most apparent difference is the location where the sleep test is performed. A home sleep test is conducted in the comfort of your own home, while a sleep test in a sleep clinic takes place in a specialized sleep center or clinic.
Equipment: In a sleep clinic, you typically spend a night in a sleep laboratory, where a variety of sensors and monitoring equipment are used to collect data while you sleep. These sensors may include electrodes to monitor brain activity (EEG), sensors to measure eye movements (EOG), sensors to assess muscle tone (EMG), and others to monitor respiratory functions, heart rate, and oxygen levels.
On the other hand, a home sleep test usually involves a more simplified set of equipment that you can take home with you. This typically includes a portable device that measures breathing patterns, oxygen levels, and heart rate. The equipment is usually less comprehensive than what is used in a sleep clinic, but it can still provide valuable data for diagnosing sleep disorders.
Convenience: Home sleep tests are generally more convenient as they allow you to sleep in your own bed and follow your regular bedtime routine. You can simply pick up the equipment from the sleep clinic, use it at home, and return it the next day. Sleep tests in a clinic require spending a night away from home and adhering to the sleep clinic's schedule.
Cost: Home sleep tests are often less expensive than sleep tests conducted in a sleep clinic. Since the equipment is simpler and the test is performed at home, it reduces the overall costs associated with the testing process.
Bruxism as symptom of OSA
Bruxism, which refers to the habitual grinding or clenching of teeth, can be associated with obstructive sleep apnea (OSA). While not all individuals with OSA experience bruxism, there is evidence to suggest a potential link between the two conditions. Here's how bruxism can be a symptom or related to OSA:
Sleep Fragmentation: OSA is characterized by repeated disruptions in breathing during sleep due to the partial or complete blockage of the upper airway. These breathing pauses can cause sleep fragmentation, leading to arousal from deep sleep stages to lighter sleep or even brief awakenings. Sleep fragmentation can contribute to the development or exacerbation of bruxism.
Micro arousals and Muscle Activation: The repetitive episodes of interrupted breathing in OSA can trigger micro arousals, which are brief awakenings that are often not fully remembered by the individual. These micro arousals can result in increased muscle activation, including the jaw muscles involved in bruxism.
Airway and Bite Alignment: OSA is associated with anatomical factors such as a narrowed or collapsible upper airway. These anatomical characteristics can also affect the alignment and positioning of the teeth and jaws. The altered bite alignment can contribute to an increased risk of bruxism.
Shared Neurological Mechanisms: Both bruxism and OSA involve alterations in the central nervous system. Certain neurological mechanisms, such as abnormalities in the regulation of sleep and wakefulness, can influence both conditions. These shared neurological factors may contribute to the co-occurrence of bruxism and OSA in some individuals.
It's important to note that not all individuals with bruxism have OSA, and not all individuals with OSA have bruxism. However, if you experience symptoms of bruxism (such as teeth grinding, jaw clenching, worn tooth surfaces, or jaw pain) along with symptoms of OSA (such as loud snoring, daytime sleepiness, witnessed breathing pauses), it may be beneficial to consult with a healthcare professional. They can evaluate your symptoms, conduct a comprehensive assessment, and determine if further evaluation for OSA is necessary, which may involve a sleep study or referral to a sleep specialist.
What is the cost difference between home sleep testing vs the sleep test in a sleep clinic?
The cost difference between home sleep testing and sleep testing in a sleep clinic can vary depending on several factors, including the specific location, healthcare provider, insurance coverage, and the complexity of the test. However, as a general trend, home sleep tests tend to be less expensive than sleep tests conducted in a sleep clinic.
Home Sleep Testing (HST): The cost of a home sleep test can range from around $150 to $500, depending on various factors. It's important to note that this cost typically covers the rental or loan of the equipment, data analysis, and interpretation of the results by a sleep specialist. Some insurance plans may partially or fully cover the cost of home sleep testing, particularly if it is deemed medically necessary.
Sleep Test in a Sleep Clinic: A sleep test conducted in a sleep clinic is generally more comprehensive and involves more sophisticated equipment and monitoring. The cost of a sleep test in a sleep clinic can range from $1,000 to $5,000 or more. This higher cost reflects the additional resources required for conducting the test in a specialized facility and the involvement of sleep technicians and healthcare professionals.
Insurance Coverage: Insurance coverage can significantly impact the out-of-pocket cost for both home sleep testing and sleep tests in a sleep clinic. It is important to check with your insurance provider to understand the specific coverage details, including deductibles, copayments, and any pre-authorization requirements.
What are oral appliances for obstructive sleep apnea
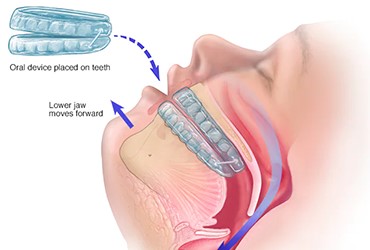
Oral appliances, also known as mandibular advancement devices (MADs) or oral mandibular repositioning devices (MRDs), are a non-invasive treatment option for mild to moderate obstructive sleep apnea (OSA) and snoring. These custom-made devices are designed to be worn during sleep and help keep the airway open by repositioning the lower jaw and tongue forward. Here are some key features and benefits of oral appliances for OSA:
Design and Function: Oral appliances are typically made of acrylic material and custom-fitted to an individual's mouth. They consist of upper and lower dental trays that fit over the teeth and are connected by a hinge or adjustable mechanisms. The lower tray is designed to advance the lower jaw slightly forward, which helps open up the airway and reduce obstruction during sleep.
Ease of Use: Oral appliances are relatively easy to use and maintain. They are comfortable to wear and do not require any external power sources, masks, or tubes like continuous positive airway pressure (CPAP) machines. They are also portable and convenient for travel.
Customization and Adjustability: Oral appliances are custom-made to fit an individual's mouth and teeth, ensuring a comfortable and secure fit. They can be adjusted and titrated by a dentist or sleep specialist to optimize their effectiveness and comfort.
Improved Sleep and Symptoms: Oral appliances can effectively treat snoring and mild to moderate OSA by improving airflow and reducing the frequency and severity of breathing disruptions during sleep. By keeping the airway open, they help alleviate symptoms such as snoring, daytime sleepiness, and fatigue.
Compliance and Patient Preference: Oral appliances offer an alternative for individuals who find it difficult to tolerate or comply with CPAP therapy. Some people prefer the convenience and comfort of wearing an oral appliance over a mask and machine.
Multidisciplinary Approach: Oral appliance therapy is often part of a multidisciplinary approach to managing OSA. Dentists work closely with sleep medicine specialists to assess the suitability of oral appliances, monitor treatment progress, and ensure optimal patient outcomes.
What are the signs of OSA
Obstructive sleep apnea (OSA) is a sleep disorder characterized by repeated episodes of partial or complete blockage of the upper airway during sleep. The signs of OSA can vary among individuals, but here are some common signs to be aware of:
Loud and Chronic Snoring: Intense and persistent snoring is often one of the prominent signs of OSA. The snoring is usually loud, disruptive, and can be accompanied by gasping or choking sounds as breathing is momentarily interrupted.
Witnessed Breathing Pauses: Bed partners or family members may witness episodes of breathing pauses during sleep. These pauses are often followed by loud snorts, gasps, or choking sounds as the individual briefly wakes up to resume breathing.
Excessive Daytime Sleepiness: Individuals with OSA often experience excessive daytime sleepiness, feeling tired and fatigued even after a full night's sleep. They may struggle to stay awake or alert during the day and may unintentionally fall asleep in inappropriate situations, such as during meetings or while driving.
Morning Headaches: Waking up with a headache or experiencing frequent morning headaches can be a sign of OSA. These headaches are often attributed to the disrupted sleep patterns and intermittent oxygen deprivation associated with the condition.
Fragmented Sleep and Insomnia: OSA can cause frequent awakenings during sleep due to breathing difficulties, resulting in fragmented and restless sleep. Individuals may find it challenging to maintain continuous sleep, leading to insomnia and feeling unrested upon waking.
Dry Mouth or Sore Throat: Breathing through the mouth due to airway blockage can lead to a dry mouth or a sore throat upon waking.
Nocturia: OSA may contribute to nocturia, which refers to the need to wake up frequently during the night to urinate. The disrupted sleep patterns associated with OSA can affect the body's regulation of fluid balance.
Daytime Fatigue and Impaired Functioning: OSA can significantly impact daytime functioning, causing excessive fatigue, irritability, mood swings, and reduced cognitive performance. Concentration, memory, and the ability to focus on tasks may be compromised.
Gasping or Choking Sensations: Some individuals with OSA may experience sudden awakenings with a feeling of gasping or choking as they struggle to breathe. This can be distressing and often leads to disrupted sleep.
Restless Sleep and Movement: Restlessness during sleep, such as tossing and turning, frequent shifts in body position, or kicking movements, can be associated with OSA. These movements may occur as the body attempts to overcome the airway blockage and restore normal breathing.
Mood and Cognitive Changes: OSA can have a significant impact on mood and cognitive function. Individuals may experience irritability, mood swings, difficulty concentrating, memory problems, and decreased cognitive performance.
When are oral appliances recommended for OSA(Obstructive Sleep Apnea)
Oral appliances, also known as mandibular advancement devices (MADs) or oral mandibular repositioning devices (MRDs), are recommended for the treatment of obstructive sleep apnea (OSA) in specific situations. The decision to recommend oral appliances is typically made by a sleep medicine specialist or dentist with expertise in sleep-related breathing disorders. Here are some common scenarios in which oral appliances may be considered:
Mild to Moderate OSA: Oral appliances are commonly prescribed for individuals with mild to moderate OSA. These are cases where the apnea-hypopnea index (AHI) or respiratory disturbance index (RDI) falls within a certain range (generally up to approximately 30 events per hour). Oral appliances are often recommended as a first-line treatment for these individuals, especially if they are unable to tolerate or prefer not to use continuous positive airway pressure (CPAP) therapy.
CPAP Intolerance or Inadequate CPAP Compliance: Some individuals with OSA may struggle with CPAP therapy due to difficulty tolerating the mask, discomfort, claustrophobia, or other reasons. In such cases, oral appliances may be recommended as an alternative treatment option to improve patient compliance and adherence.
Combination Therapy: In certain situations, oral appliances may be used in combination with other treatment modalities for OSA. For example, individuals who are already using CPAP but experience persistent residual sleep apnea or persistent snoring despite adequate CPAP pressure may benefit from adjunctive use of an oral appliance to further improve outcomes.
Anatomical Considerations: The anatomical characteristics of an individual's upper airway and jaw structure can influence the suitability of oral appliance therapy. Oral appliances are generally more effective in individuals with specific anatomical features, such as a well-defined dental arch, healthy teeth, and a normal body mass index (BMI).
Patient Preference: Patient preference and willingness to use oral appliances play a role in the decision-making process. Some individuals may prefer the comfort, convenience, and portability of oral appliances over CPAP therapy, leading to the recommendation of oral appliance therapy as a suitable treatment option.
Why does your dentist recommend a sleep test?
Your dentist may recommend a sleep test for several reasons related to oral health and potential sleep-related breathing disorders. Here are some common reasons why a dentist may suggest a sleep test:
Assessment of Sleep-Related Breathing Disorders: Dentists are often the first healthcare professionals to identify signs or symptoms of sleep-related breathing disorders, such as obstructive sleep apnea (OSA). These disorders can have oral health implications, such as teeth grinding (bruxism), dry mouth, and temporomandibular joint (TMJ) disorders. A sleep test helps confirm the presence and severity of these disorders, guiding appropriate treatment.
Evaluation of Oral Appliance Therapy Suitability: Oral appliances, such as mandibular advancement devices, can be effective in managing mild to moderate cases of sleep apnea and snoring. However, before prescribing an oral appliance, it is essential to confirm the diagnosis through a sleep test. The sleep test helps determine if an oral appliance is a suitable treatment option for the patient.
Collaborative Care with Sleep Specialists: Dentists often work in collaboration with sleep medicine specialists and other healthcare providers to manage sleep-related breathing disorders. By recommending a sleep test, the dentist ensures that accurate diagnostic information is available for a comprehensive evaluation and treatment planning. The results of the sleep test guide the dentist and sleep specialist in developing an appropriate treatment approach.
Monitoring Treatment Outcomes: If a patient is undergoing treatment for sleep-related breathing disorders, such as using an oral appliance or continuous positive airway pressure (CPAP) machine, periodic sleep tests may be recommended to monitor the effectiveness of the treatment. The sleep test provides objective data on treatment outcomes and helps make adjustments as needed.
Why do patients coming to dental office need to be sleep tested?
Patients coming to a dental office may be recommended to undergo a sleep test if their dentist suspects that they have a sleep-related breathing disorder, such as obstructive sleep apnea (OSA). Dental professionals are increasingly involved in the screening and management of sleep disorders due to their close proximity to the oral and craniofacial structures, which can contribute to sleep-disordered breathing.
Here are a few reasons why patients coming to a dental office may need to be sleep tested:
Symptoms: Patients who report symptoms such as chronic snoring, excessive daytime sleepiness, gasping or choking during sleep, morning headaches, and frequent awakenings may be showing signs of a sleep-related breathing disorder. A sleep test can help determine the presence and severity of these conditions.
Oral and Craniofacial Examination: Dentists can identify certain anatomical features that can contribute to sleep-related breathing disorders. These features include a narrow or crowded upper airway, enlarged tonsils or adenoids, a large tongue, or a small jaw. By assessing these factors, dentists can determine if a sleep test is necessary.
Oral Appliance Therapy: Oral appliances, such as mandibular advancement devices, can be an effective treatment for mild to moderate obstructive sleep apnea. Before prescribing an oral appliance, it is important to confirm the diagnosis through a sleep test to determine the appropriate treatment approach.
Collaborative Care: Dentists often work in collaboration with sleep medicine specialists and other healthcare providers to manage sleep-related breathing disorders. A sleep test provides objective data that helps guide treatment decisions and facilitates effective interdisciplinary care.
Treatment Monitoring: Sleep tests may also be recommended to monitor the effectiveness of treatment interventions. For example, if a patient with sleep apnea is using a continuous positive airway pressure (CPAP) machine or an oral appliance, periodic sleep tests can assess treatment outcomes and make necessary adjustments.