Traumatic Occlusion

Traumatic Occlusion
This article aims to emphasize the role of early detection of occlusal trauma and thereafter providing orthodontic treatment to prevent further damage to periodontium and loss of dental structures. Many a times, the role of occlusion in trauma from occlusion is neglected, which can hamper early diagnosis and intervention.
Our Teeth have Cusps and fissures. When the upper and lower teeth come together like puzzle pieces, there should be a harmonious closure of the bite. This inter-cuspation of teeth is called an occlusion. An improper occlusion is called a malocclusion. A proper occlusion ensures not only proper distribution of biting forces, but also the normal tense and flex of the muscles that are attached to the jaws.
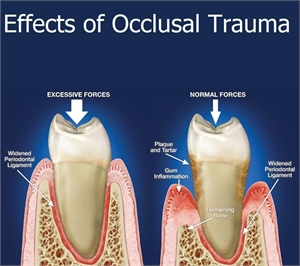
Each tooth is surrounded by a complex tissue system known as the periodontium. This periodontium constitutes the gingiva, the underlying bone (alveolar bone), the ligament (periodontal ligament) connecting the tooth and the bone, and the hard tissue covering the roots (cementum). It is because of the periodontium that each individual tooth is able to bare and resist the various forces acting upon them. However, there are cases when an improper force, arising due to the bite causes damaging changes in the periodontium. This is called occlusal trauma.
Trauma to the teeth arising as a result of improper occlusion can be grouped into two types: Primary and Secondary.
Primary occlusal trauma is when there is absence of a periodontal disease or condition. It arises because of parafunctional habits like clenching or grinding teeth (bruxism), chewing upon fingernails, pens, pencils, etc. The duration, frequency and magnitude of these habits directly correspond to the damage on the tooth.
Secondary occlusal trauma is when occlusal forces exaggerate the damage on a tooth that is already having a periodontal condition or disease.
Cause of primary occlusal trauma:
otherwise healthy state, the reason for the trauma can be due to a malocclusion like a deep bite, where upper teeth overlapping the lower teeth lay down heavy forces on normal closure of the mouth.
Occlusal trauma has been defined as injury to the periodontium resulting from occlusal forces that exceeds the reparative capacity of the attachment apparatus. Trauma from occlusion refers to tissue injury due to distorted occlusion. An occlusion that produces such injury is called a traumatic occlusion. Acute trauma from occlusion can result from an abrupt occlusal impact on bitten objects, restorations or prosthetic appliances that interfere with or alter the occlusal forces on teeth.
Chronic trauma from occlusion is more common than acute trauma and develops from gradual changes in occlusion produced by tooth wear, drifting movement, extrusion of teeth, combined with parafunctional habits such as bruxism and clenching.
Trauma from occlusion is considered the primary etiological factor, and the only local alteration to which a tooth is subjected is from occlusion. Secondary trauma from occlusion occurs when the adaptive capacity of the tissues to withstand occlusal forces is impaired by bone loss resulting from marginal inflammation. The periodontium becomes more vulnerable to injury, and previously well-tolerated occlusal forces become traumatic.
Occlusal trauma can also arise because of over-eruption of one tooth of the opposing arch.
Malocclusion
Grinding of teeth(bruxism) can cause occlusal trauma.
Recent dental treatments, wherein a tooth is restored with a restorative material can also contribute to occlusal trauma if the restoration is done higher than the normal occlusal level.
Signs and symptoms of occlusal trauma
Mobile teeth is the most common sign of a tooth that has occlusal trauma. It occurs because of a condition called fremitus. This is basically when the tooth exhibits mobility caused due to widening of the ligament surrounding it that primarily occured because of undue forces of occlusion.
A tooth whose periodontal condition becomes compromised might as well rotate or drift away from its normal position in the oral cavity.
Pain and sensitivity are common findings arising as a result of excessive forces.
TMJ pain with muscle tenderness around the jaw.
Regular and consistent occlusal forces that lead to trauma can also lead to the tooth's surface become gradually chewed away leading to the formation of wear facets.
Diagnosis of occlusal trauma
The diagnosis and assessment of occlusal trauma is not merely made based on a single examination, due to the necessarily progressive nature of injury. Orthodontic correction is usually restricted to cases where tooth malpositions are the prime cause of trauma.
Clinically, the patient is asked to close his or her mouth and a suspected occlusal trauma can be diagnosed by observing the intercuspation of teeth. Gingival bleeding around the affected tooth can be seen. The excessive traumatic force can devoid the tooth of blood supply. A radiograph is taken to understand the extent of resorption of the underlying bone and subsequent widening of the periodontal ligament.